So you’ve just started antibiotics and you’re wondering how long does it take for the antibiotics to work—and honestly, that’s the right question to ask. Most people expect to feel better overnight, but the reality is a bit more nuanced. The timeline depends on several factors including the type of infection, the antibiotic prescribed, and your body’s response. Let’s break down what you actually need to know.
Table of Contents
Typical Timeline for Relief
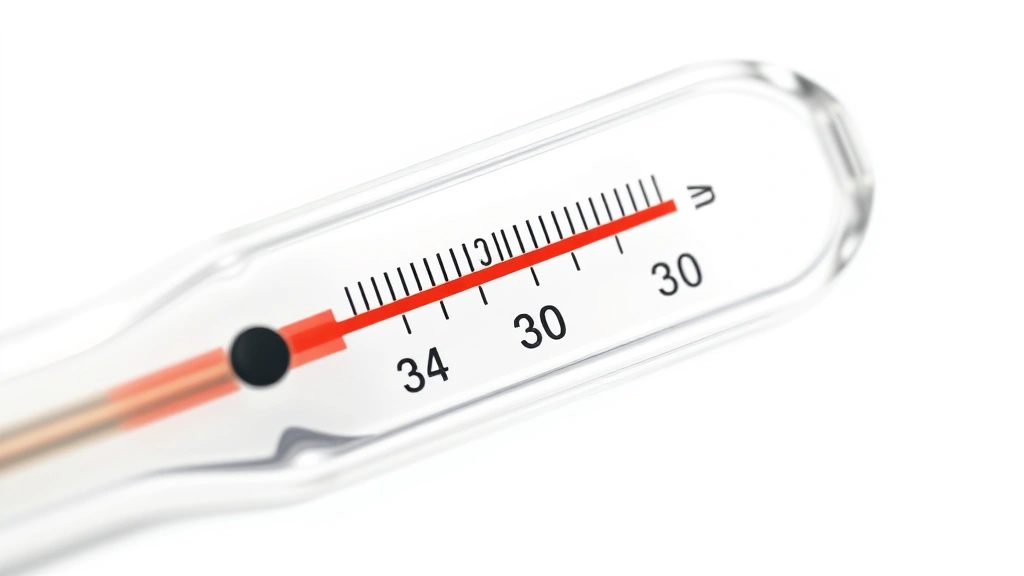
Here’s the straightforward answer: most antibiotics start working within 24 to 48 hours, but you might not feel dramatically better immediately. Your body needs time to clear out the bacteria and repair the damage they’ve caused. For bacterial infections like strep throat or urinary tract infections, you’ll typically notice improvement in symptoms within 2-3 days. However, some infections take longer—pneumonia might require a full week before you feel significantly better.
The key thing to understand is that antibiotics work on two timelines: the bacterial timeline and the symptom timeline. The antibiotic starts killing bacteria right away, but your body’s inflammatory response—the stuff causing your pain, fever, and fatigue—takes longer to calm down. Think of it like turning off a fire: the antibiotics stop the flames from spreading, but the embers still need time to cool.
Factors Affecting Speed
Several variables determine how quickly you’ll feel better. Your immune system strength matters significantly—people with compromised immunity might see slower improvement. The severity of your infection plays a huge role too. A mild ear infection responds faster than a serious sinus infection or bronchitis. Your overall health, age, and whether you’re taking the antibiotic consistently all impact the timeline.
Dosage and frequency matter more than most people realize. If you’re taking the antibiotic exactly as prescribed, you’ll see faster results than if you’re skipping doses or taking it irregularly. Your body weight and metabolism also influence how quickly the medication reaches therapeutic levels in your system. Even something like whether you take the antibiotic with food or on an empty stomach (depending on the specific drug) can affect absorption rates.
Different Antibiotic Types
Not all antibiotics work at the same speed. Penicillin-based antibiotics like amoxicillin typically show results within 24-48 hours for common infections. Fluoroquinolones (like Cipro) often work faster, sometimes showing improvement within 12-24 hours. Macrolides like azithromycin (Z-pack) fall somewhere in the middle, usually 24-36 hours. Cephalosporins are generally quick-acting, similar to penicillins.
The mechanism matters too. Bactericidal antibiotics (which kill bacteria directly) show faster symptom relief than bacteriostatic ones (which stop bacteria from multiplying). Your doctor chooses the antibiotic based on the specific bacteria causing your infection, so different infections get different drugs—which means different timelines. This is why it’s crucial not to use leftover antibiotics from a previous infection.
Signs It’s Actually Working
You don’t need to wait for complete symptom disappearance to know it’s working. Within 24-48 hours, watch for subtle improvements: your fever might drop slightly, your energy might increase a bit, or the pain might become less sharp. These are signs the antibiotic is doing its job. Your body might also show signs of fighting the infection—some people experience mild flu-like symptoms as their immune system responds to dead bacteria.
More obvious signs come around day 3-5: you can breathe easier if you had respiratory infection, your throat feels less raw, or your urinary symptoms improve significantly. The key is that improvement should be noticeable by day 3. If you’re on antibiotics and feeling exactly the same on day 4, that’s when you contact your doctor. It could mean the antibiotic isn’t right for your infection, or you might have a viral infection that antibiotics won’t touch.
When to Worry or Call Doctor
You should contact your doctor immediately if you develop new symptoms while on antibiotics, experience severe allergic reactions (rash, swelling, difficulty breathing), or if your original symptoms worsen after 48 hours. Also reach out if you notice signs of a secondary infection—antibiotics can sometimes allow yeast infections to develop because they kill beneficial bacteria too.

Don’t panic if you’re not miraculously better by day 2. But do call if you’re showing zero improvement by day 4, or if you experience severe side effects like persistent diarrhea, severe nausea, or unusual symptoms. Your doctor might need to switch you to a different antibiotic or investigate whether something else is going on. Some infections are trickier than others, and sometimes the first antibiotic prescribed isn’t the perfect match.
Maximizing Antibiotic Effectiveness
Take your antibiotic exactly as prescribed—same time each day, same dosage, no skipping doses. Set phone reminders if you’re forgetful. Don’t stop taking it early just because you feel better; finishing the full course is critical for preventing antibiotic resistance and ensuring the infection doesn’t come roaring back. Typically you need to take antibiotics for 7-10 days, sometimes longer depending on the infection.
Support your body’s healing process by staying hydrated, getting adequate sleep, and eating nutritious food. If you’re dealing with a respiratory infection, similar to how you’d want proper ventilation when preparing your kitchen, you’ll want good air quality and humidity levels in your space. Avoid smoking and secondhand smoke, which can slow recovery. If your antibiotic causes stomach upset, ask your doctor if you can take it with food—some antibiotics absorb better with meals, others on an empty stomach.
Common Mistakes People Make
The biggest mistake is stopping antibiotics early. You feel better on day 4, so you think you’re done—but you’re not. Stopping early leaves behind resistant bacteria that can cause a relapse, sometimes worse than the original infection. This is how antibiotic-resistant superbugs develop, and it’s a serious public health issue.
Another common error is not taking it consistently. You miss a dose here, take it at different times there, and suddenly the medication levels in your bloodstream drop too low to be effective. You also shouldn’t share antibiotics with family members or use old antibiotics from previous infections. Just because you had a similar infection before doesn’t mean the same antibiotic will work this time. Your body’s natural recovery process is like maintaining health habits—consistency matters more than intensity, much like how regular care beats emergency intervention.
Recovery Expectations
Complete recovery timelines vary widely. For simple infections like strep throat, you might feel 90% better within 5-7 days. More serious infections like pneumonia can take 2-3 weeks for full recovery, even though you’ll feel much better within the first week. Some infections leave you feeling fatigued for weeks after the antibiotics finish—that’s normal as your body repairs tissue damage and replenishes energy stores.
Expect that you might still have mild symptoms even after the antibiotic course ends. A lingering cough after bronchitis or slight throat soreness after strep is common and usually resolves within a few more days. However, if major symptoms return after you’ve finished the antibiotics, contact your doctor—you might need a different treatment or there could be complications.
Frequently Asked Questions
Can I stop taking antibiotics once I feel better?
No. You must complete the full course even if you feel better after a few days. Stopping early allows remaining bacteria to survive and multiply, potentially causing a worse infection and contributing to antibiotic resistance. Your doctor prescribes a specific duration for a reason.
Why aren’t antibiotics working for my infection?
Several reasons: the infection might be viral (antibiotics only work on bacteria), you might have antibiotic-resistant bacteria, the dosage might be too low, or the specific antibiotic might not be right for your infection. Contact your doctor if you’re not improving by day 4. They can test to identify the exact bacteria and potentially switch your medication.
How long after starting antibiotics am I contagious?
For most bacterial infections, you become non-contagious within 24 hours of starting the right antibiotic. However, follow your doctor’s guidance on returning to work or school—some infections require longer isolation periods. For strep throat specifically, you’re typically safe to return after 24 hours on antibiotics.
Do antibiotics work faster if I take more than prescribed?
No. Taking more than prescribed won’t speed up recovery and significantly increases your risk of serious side effects. The dosage your doctor prescribes is calculated based on your weight, age, and the infection type. More isn’t better—it’s just dangerous.
What should I do about side effects?
Common side effects like mild nausea or stomach upset often improve after a few doses. Taking the antibiotic with food (if appropriate for that specific drug) can help. However, serious side effects like severe allergic reactions, severe diarrhea, or unusual symptoms warrant immediate medical attention. Don’t just stop taking it—call your doctor.
Can I drink alcohol while taking antibiotics?
Most antibiotics are safe with moderate alcohol consumption, but some (like metronidazole) have serious interactions. Check with your pharmacist or doctor about your specific antibiotic. Even when it’s technically safe, alcohol can dehydrate you and slow your recovery, so it’s wise to avoid it while fighting an infection.
Why do I still feel tired after finishing antibiotics?
Your body has been fighting infection and working hard to heal tissue damage. Recovery fatigue is completely normal and can last days or even weeks after you finish antibiotics. Continue resting, eating well, and staying hydrated. If fatigue persists beyond a few weeks, contact your doctor to rule out complications.
Conclusion
Understanding how long does it take for the antibiotics to work helps you manage expectations and recognize when something might be wrong. Most antibiotics start working within 24-48 hours, with noticeable symptom improvement by day 3-5. However, the exact timeline depends on your infection type, the specific antibiotic prescribed, your immune system strength, and how consistently you take the medication. The most important thing you can do is take your antibiotics exactly as prescribed, complete the full course even when you feel better, and contact your doctor if you’re not improving by day 4 or if you experience concerning side effects. Your body’s healing process takes time, but with proper antibiotic use and supportive care, most infections resolve successfully.
For more information on health timelines and recovery processes, check out authoritative resources from the CDC on antibiotic use, the Mayo Clinic, and WebMD’s medical resources. These sources provide evidence-based information about infection treatment and recovery expectations.